Northern California Achilles Tendon Injuries

Introduction
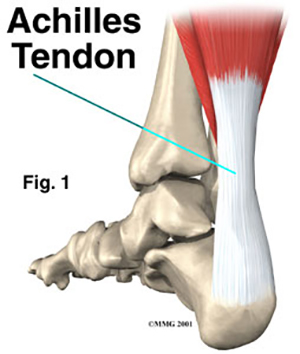
Problems that affect the Achilles tendon (Fig. 1) are common among active middle-aged people. These problems cause pain at the back of the calf and may result in a rupture of the Achilles tendon in severe cases.
Anatomy
The Achilles tendon is a strong, fibrous band that connects the calf muscle to the heel. The calf is actually formed by two muscles, the underlying soleus and the thick outer gastrocnemius (Fig. 2). These muscles form the gastroc-soleus muscle group.
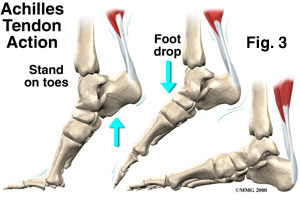
During contraction, these muscles pull on the Achilles tendon causing your foot to point down and helping you rise on your toes (Fig. 3). This powerful muscle group helps in sprinting, jumping, and climbing.
Several different problems can occur that affect the Achilles tendon, some rather minor and some quite severe.
Tendocalcaneal Bursitis
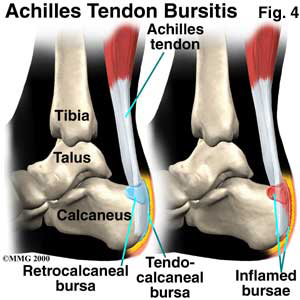
A bursa is a fluid filled sac designed to limit friction between rubbing parts. These sacs are found in many places in the body. When a bursa becomes inflamed, it is called bursitis (Fig. 4). Tendocalcaneal bursitis is an inflammation in the bursa behind the heel bone.
Achilles Tendonitis
A major strain can cause injury to the calf muscles or the Achilles tendon. This can happen during a strong contraction of the muscle, as when running or sprinting. Landing on the ground after a jump can force the foot upward causing injury. The injury can affect different portions of the muscles or tendon. The injury may occur in the center of the muscle or it may happen where the muscles join the Achilles tendon (called the musculotendinous junction). Chronic overuse may contribute to changes in the Achilles tendon as well, leading to degeneration and thickening of the tendon.
Achilles Tendon Rupture
In severe cases, the force of a major muscle strain may even rupture the tendon. The classic example is a weekend athlete who places too much stress on the tendon and experiences a tearing of the tendon (Fig. 6). In some instances, an achilles tendon rupture may be preceded by a period of tendonitis, which makes the tendon weaker than normal.
Causes
Problems with the Achilles tendon seem to occur in different ways. Initially, irritation of the outer covering of the tendon, called the paratenon, causes a paratendonitis. Paratendonitis is simply inflammation around the tendon. Inflammation of the tendocalcaneal bursa may also be present with paratendonitis. Either of these conditions may be due to repeated overuse or ill-fitting shoes that rub on the tendon or bursa.
As we age, our tendons can degenerate. Wear and tear occurs in the tendon and weakens it. Degeneration usually appears as a loss of the normal tendon fiber arrangement. Tendons are made up of strands of a material called collagen. (The structure of a tendon is similar to a rope.) Some of the individual strands of the tendon can become jumbled due to the degeneration (Fig. 7), other fibers break, and the tendon loses strength.
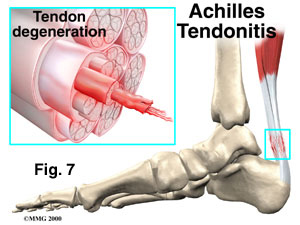
The healing process thickens the tendon as scar tissue builds up. This can continue until nodules are formed within the tendon. This condition is called tendinosis. The weakened, degenerative tendon may lead to a rupture of the Achilles tendon.
Symptoms
Tendocalcaneal bursitis usually begins with pain and irritation at the back of the heel (Fig. 8). Redness and swelling may occur. The back of the shoe may further irritate the condition, making it difficult to tolerate shoe wear.
Achilles tendonitis usually occurs further up the leg, just above the heel bone itself (Fig. 8). The Achilles tendon may be noticeably thickened and tender to the touch. Pain may be present with walking, especially when pushing off on the toes.
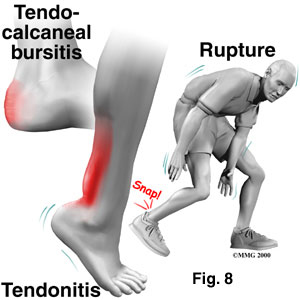
An Achilles tendon rupture is usually an unmistakable event. A snapping noise may be heard when the Achilles tendon ruptures (Fig. 8). The rupture may feel similar to being kicked in the calf. Following rupture the calf may swell, and the injured person usually can’t rise on his toes.
Diagnosis
Diagnosis is made through physical examination and consideration of the patient’s medical history. If it is uncertain whether the Achilles tendon has been ruptured, an MRI (magnetic resonance imaging) scan may be necessary to confirm the diagnosis. The MRI machine uses magnetic waves rather than X-rays to show the soft tissues of the body. This machine creates images that look like slices of the area your doctor is interested in and shows the tendons and ligaments very clearly. This test does not require any needles or special dye and is painless.
Treatment
Conservative Treatment
Non-surgical treatment for tendocalcaneal bursitis and Achilles tendonitis usually starts with a combination of rest, anti-inflammatory medications such as aspirin or ibuprofen, and physical therapy. Several physical therapy treatments may be available in the early stages of Achilles tendonitis or tendocalcaneal bursitis.
Ice
Ice can be used after tendocalcaneal bursitis, Achilles tendonitis and to calm an inflamed bursa. Initially, a patient should ice fifteen minutes every hour. A doctor may recommend a cold temperature whirlpool. The cold water helps reduce swelling and pain, and the moving water in the whirlpool provides a massage action. In supervised physical therapy, a therapist may continue treatments with ice bags, cold packs, or ice massages.
Rest
These types of injuries usually require rest. Activities like walking on the sore leg should be limited. Small (one-quarter inch) heel lifts can minimize stress by putting slack in the calf muscle and Achilles tendon. Similar sized heel lifts should be placed in both shoes to keep everything aligned.
A cortisone injection is not advised for tendocalcaneal bursitis and Achilles tendinitis. Following cortisone injections there is an increased risk of tendon rupture.
Treatment of an Achilles tendon rupture with a cast will allow the vast majority of tendon ruptures to heal. However, the incidence of re-rupture is increased in those patients treated with casting. In addition, the strength of the healed tendon is significantly less in patients treated with a cast.
Surgery
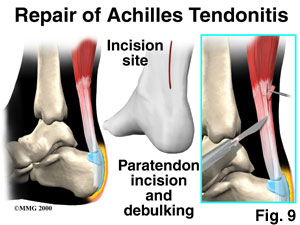
Surgical treatment for Achilles tendonitis is not usually necessary for most patients. However, in some cases of persistent tendonitis and tendinosis a procedure called debulking of the Achilles tendon may be performed.
This procedure is usually done through an incision on the back of the ankle near the Achilles tendon. The tendon is identified, and any inflamed paratenon tissue (the covering of the tendon) is removed. The tendon is then split, and the degenerative portion of the tendon is removed (Fig. 9). The split tendon is then repaired and allowed to heal. Removing the degenerative portion of the tendon stimulates repair of the tendon to a more normal state.
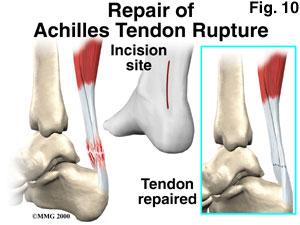
Surgery may also be suggested for treatment of a ruptured Achilles tendon. Re-attaching the two ends of the tendon repairs the torn Achilles tendon (Fig. 10). This procedure is usually done through an incision on the back of the ankle near the Achilles tendon. Numerous procedures have been developed to repair the tendon. Most procedures involve sewing the two ends of the tendon together. Repair techniques have been developed to minimize the size of the incision.
Rehabilitation
After surgery, a cast or brace will be used to protect the repair and the skin incision. The cast or brace may be required for six to eight weeks. Following removal of the cast, a shoe with a high heel may be worn for several weeks. Physical therapy may be recommended for regaining full motion of the ankle and strength in the calf muscles.
